As fears mount globally about mpox, apparently simple questions such as the danger it poses and differences between variants do not have clear and simple answers.
The World Health Organisation in July declared an international health emergency over the spread of mpox, which first appeared in humans around 1970 in the Democratic Republic of Congo (DRC).
For decades, the illness long known as "monkeypox" was restricted to a handful of African countries, with estimates of its mortality rate ranging from one to 10% of people infected.
That uncertainty grew from 2022, when mpox spread elsewhere in the world, especially to Western countries.
Cases in these newly-infected states had very low mortality of around 0.2%.
Such differences likely stem from several variables.
First, someone living in the US or Europe is much more likely to receive swift, appropriate medical treatment than patients in most African nations.
The danger mpox presents "strongly depends on the quality of basic care," said Antoine Gessain, a virologist specialising in the disease.
The mortality rate measured in the current outbreak -- around 3.6 percent -- would therefore likely be much lower were it not mostly limited to the DRC.
- Child malnutrition -
Other factors weighing on the mortality rate include those that make some patients more vulnerable than others.
The vast majority of the deaths recorded in the DRC -- over 500 out of more than 15,000 mpox cases -- have been children, many of whom are affected by malnutrition in the country.
By contrast, in the DRC's 2022-23 epidemic, the very small number of people who died -- around 200 out of 100,000 cases -- were mostly adults whose immune system was already weakened by HIV infection.
Different mortality outcomes can also be explained by the way a disease is spread.
In 2022-23, most transmission was via sex between homosexual or bisexual men.
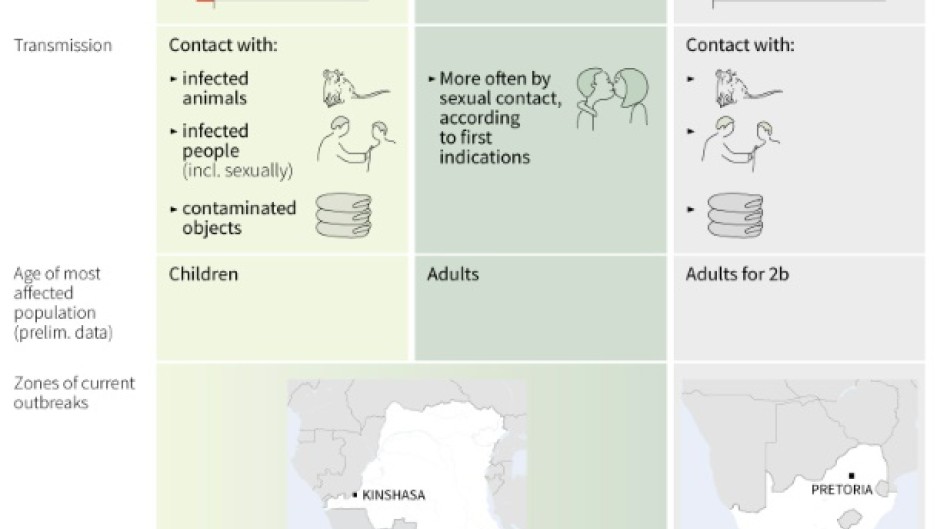
A further factor adding complexity is the clade, or family, to which the specific virus causing an mpox outbreak belongs.
Scientists are struggling to determine the differences between clades when it comes to health risks and transmission.
- Tricky comparisons -
The 2022-23 mpox epidemic was caused by Clade 2 mpox, which is mostly present in western Africa, but also found in South Africa.
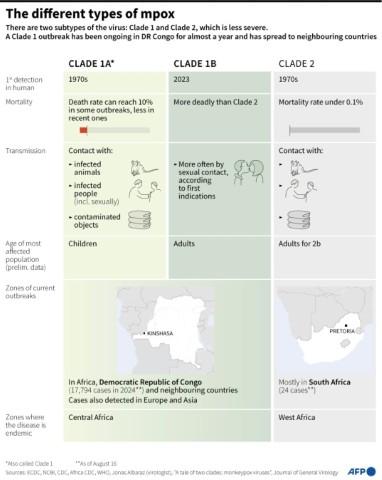
DRC's deadly current outbreak stems from Clade 1 mpox, mostly found in the continent's central areas.
But a distinct second epidemic hitting mostly adults in the same country is linked to variant 1b, a derivative of Clade 1 that has only appeared recently.
Confusion in the media has led some outlets to call variant 1b more dangerous than previously-existing mpox varieties.
"There are rather big claims in the popular media for which evidence is limited, both about severity and about transmissibility of the new sublineage 1b," Dutch virologist Marion Koopmans told the UK-based Science Media Centre.
"What we do know is that Clade 1 is associated with more severe disease than Clade 2," she added.
In the past, Clade 1 outbreaks have been associated with higher mortality rates than Clade 2.
But researchers call for caution before drawing conclusions, even with apparently clear-cut figures.
The urgency of establishing the facts about mpox variants is all the greater as Clade 1 was detected in Sweden in mid-July -- for the first time outside Africa.
"It's very difficult to compare" between different clades "given that the context and the type of at-risk population are so important," virologist Gessain said.
"How can you compare children suffering from malnutrition and HIV-positive adults?" he asked.
By Julie Pacorel